Equipment / Instruments
Unit 10: Cleaning & Sterilizing
Topic 3: Sterilizing Techniques
Sterilizing & Disinfecting techniques (†most commonly used) for instruments and equipment include:
Heat
- steam†
- moist heat (boiling)
- dry heat
Irradiation
- Gamma irradiation
- High energy electrons – unavailable in Australia.
Gaseous
- Ethylene oxide
- Formaldehyde
- Gas plasma (hydrogen peroxide vapour)†
Chemical disinfectants
- Alcohols (ethyl, isopropyl)
- Aldehydes (formaldehyde & ortho-phthalaldehyde)†
- Chlorhexidine
- Iodophors
- Phenols
- Quaternary ammonium compounds.
- Peracetic acid
Heat
Heat usually destroys microbes and spores by the denaturation of cellular proteins. There is no one temperature at which all microbes and spores are destroyed, the thermal destruction of bacteria also being time and temperature-dependent.
Dry Heat
Dry heat destroys organisms by causing oxidative destruction of bacterial protoplasm. Only a few materials can be sterilized in this manner, materials such as fabrics, rubber and plastics are easily damaged. It may be used for glassware cutting instruments, ophthalmic instruments drill bits, powders and oils.
Hot air ovens must operate at a high temperature, in the range of 150-180oC to fully sterilize.
Moist Heat (Boiling)
Boiling is not a true sterilant as it may not kill all microorganisms and spores as the maximum temperature only reaches 100oC.
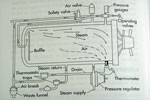
Steam Sterilization (commonly called Autoclaves)
When moisture is present, bacterial death occurs at a lower temperature in a shorter time than in an air oven (eg. Bacterial spores killed after 12 minutes exposure to steam at 120oC will require an hour in a hot air oven at 160oC).
Sterilization with saturated steam under pressure (At sea level, temperatures >100oC can only be achieved under pressure) is the most dependable and most widely used method used for sterilizing most reusable instruments and packs.
Pressure vessels (autoclaves) are relatively cheap, available in most practices and simple to use. They achieve high temperatures with dry saturated steam which is steam which does not produce water droplets on contact with materials.
Dry steam is able to penetrate porous articles and packs to give up its latent heat as condensation.
Instruments and materials such as stainless steel instruments, drapes, gowns, swabs, most rubber articles, glassware and some heat stable plastics can safely be steam sterilized.
Older style fibreoptic endoscopes, lenses and some plastics may however be damaged by this form of sterilization.
There are two main types of autoclaves available which differ in the method by which the air is removed.
- Upward displacing autoclaves function in a similar way to a pressure cooker in which water is boiled in the bottom of the closed autoclave and the air vented at the top which is then closed, allowing the pressure to build up once all of the air has been removed. However as steam is lighter than air, there is the chance of some air being trapped under a layer of steam, reducing the efficiency of the sterilizing function, and rendering the load non-sterile.
- Downward displacing autoclaves are the best and most commonly used type of steam sterilizer. Steam is introduced under pressure at the top of the sterilizing chamber, compressing the air to the bottom where it is vented to the outside. Once the air is eliminated, the valve allowing the air to be expelled is closed and the pressure and temperature rises.
Some more sophisticated autoclaves use a vacuum pump to evacuate air from the chamber before the steam is admitted. This eliminates the time lag required in gravity displacing autoclaves, and reduces the chance of air entrapment within packs. These are pre-vaccum sterilizers.
The majority of downward displacement autoclaves are also "jacketed". Jacketed autoclaves have an outer steel wall surrounding the sterilizing chamber. This jacket is used to hold prepared steam, ready for the process to start.
Residual air present in steam sterilizers (autoclaves) will reduce their efficiency significantly by limiting the diffusion of steam and its condensation.
Some autoclaves use a steam pulsing system to assist in the evacuation of air without the need for a high vacuum system. (the Pre-Vacuum type).
Steam sterilizers must have a efficient drying cycle as any packs of drapes or instruments left damp at the end of the sterilizing cycle will allowing microorganisms to penetrate porous wraps by a wicking effect.
The safe minimum time-temperature standard for the routine sterilizing of small packs is 12 minutes at 121oC and 101kPa (15 psi). Emergency sterilizing can be carried out at 134oC and 203kPa (27 psi) for 4 minutes. Added to this time is the steam penetrations time and drying time.
Total sterilizing time includes the specified sterilizing time, plus another half of that time as a safety margin, plus penetration time, plus drying time. Sterilizer technicians can advise on penetration time when servicing is done.
Irradiation
Ultra-violet light
Ultra-violet light is not a true sterilent, and is no longer used for this purpose.
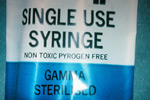
Gamma irradiation
Gamma irradiation is the most effective of these methods.
It is usually used to sterilize many pre-packaged materials such as synthetic suture materials, plastic catheters and syringes. Gamma rays do discolour glass so is not used on endoscopes.
Gaseous sterilization
Ethylene oxide
Ethylene oxide is capable of destroying all known bacteria, spores, fungi and many of the larger viruses by inactivating cellular DNA and preventing cell reproduction.
It is however extremely toxic, irritant to tissues, carcinogenic and inflammable, and sterilized materials must be aerated for at least 7 days, or in an aerator for 12-18 hours prior to use..
Its use is now restricted to fewer and fewer large sterilizing units. Because of the problems associated with its use it is only used to sterilize instruments which may be damaged by heat sterilization.
Gas plasma
Gas plasma (low temperature hydrogen peroxide vapour) is a more recent innovation which a gas plasma is generated by application of a radiofrequency waves (13.56 Mhz) to the vapour of hydrogen peroxide at 42oC.
The ensuing reaction denatures the cellular DNA and RNA. The by-product of the reaction is water and oxygen and is therefore relatively harmless.
Gas plasma sterilization is now available in many larger human hospitals. A fully automated system is called the “Sterrad” Sterilization System.
The entire sterilization cycle takes 75 minutes.
The gas plasma however is absorbed and neutralized by water and cellular-based materials. It is therefore incompatible with linen, paper-based wraps, liquids and metals.
Chemical High Level Disinfection
Instruments may be soaked in disinfectant solutions. This method will produce medium to high level disinfection rather than sterility.
A 2% buffered aqueous solution of glutaraldehyde (Cidex) is commonly used for the sterilization of lensed instruments such as endoscopes. This solution is bactericidal and virucidal in 20 minutes, and may be sporicidal in 3 hours. Glutaraldehyde is however extremely irritant to tissues, and instruments sterilised in this manner must be rinsed in sterile saline before use.
The use of glutaraldehyde is no longer recommended because of health and safety concerns.
Cidex OPA (ortho-phthalaldehyde)
Cidex OPA (ortho-phthalaldehyde) is a replacement for Cidex, and is less irritant, although some allergic reactions have been reported. It is a high level disinfectant for sterilizing heat sensitive equipment and is effect in 12 minutes at 20oC. It may be sporicidal.
It is essential to read the directions for use carefully, and equipment should still be rinsed prior to use.
The minimum effect concentration (MEC) of Cidex OPA is 0.3%. This solution can be re-used for up to 14 days if maintained at 25oC.

Australian Standard 4187, 2003. Cleaning, Disinfecting and Sterilizing of reusable medical and surgical instruments and equipment, and maintenance of associated environments in Healthcare facilities.
Link to download Adding value in the surgical setting. C. Bradley.pdf (168Kb)

Instrument handling