The Patient
Unit 6: Intraoperative Considerations
Topic 1: Tissue Handling
Tissue viability is a valuable adjunct to the prevention of infection and ensures rapid wound healing. It is, therefore, of the utmost importance to preserve tissue viability by proper and skilful tissue handling.
Tissue viability is mainly determined by blood supply.
You can very effectively diminish blood supply and hasten cell death by:
- rough tissue handling
- improper use of instruments
- prolonged exposure.

One of the golden rules of tissue handling is to: “Do no harm – kill as few cells as possible”.
A number of factors will influence the degree of tissue injury:
1. A knowledge of surgical anatomy
To minimize tissue injury and maintain function it is also better to make operative approaches through natural tissue planes where possible. A thorough knowledge of regional anatomy is also important in order to protect vital structures eg. nerves, major blood vessels in the surgical site.
For example, elastic loops (Neoloops) or polyester tape can be used to retract vessels and nerves from the surgical field to avoid iatrogenic injury.
2. Careful dissection.
Surgical dissection is employed to separate tissues in order to gain exposure to a body cavity or structure. Blunt dissection is the separation of tissues along natural lines of cleavage such as fascial planes using a blunt instrument or finger. In sharp dissection the separation is achieved using a scalpel or scissors. More commonly a combination of sharp and blunt dissection is employed.
Sharp dissection usually by scalpel of discrete organs eg. skin, liver, intestine, is the least traumatic technique to divide tissues. A scalpel is the standard soft tissue cutting instrument.
Scalpels (Unit 9)
Blunt dissection is safer when dissecting around vital structures, tissue planes or when normal anatomy needs to be distorted.
Scissors can be used for sharp and blunt dissection. In addition to its cutting action, the scissor blades can be used to bluntly separate tissues. With the blades closed, the tip of the scissors is introduced between tissues and the blades are gently opened. The scissors is withdrawn from the separated tissues with the blades kept apart to avoid inadvertently cutting any tissue. This is repeated several times to sequentially increase the separation between the tissues. Haemostatic forceps can be used in a similar manner for blunt dissection. Some forceps such as right-angled forceps are particularly suited for blunt dissection around blood vessels such as a patent ductus arteriosus.
3. Dissection under gentle traction
Traction applied to tissues and organs can help in the visualization of tissue planes and subsequent dissection.
Traction can be achieved by finger pressure or by retraction with appropriate instruments designed for grasping or retracting tissues.
Surgical manipulation of tissues by hand or instrument howver always produces tissue trauma. This trauma can be minimised by using appropriate instruments for specific tissues, avoiding excessive force to hold tissues, applying instruments on tissues only for the required period of holding, and avoiding repeated re-grasping of tissues. Instruments for grasping have different designs, which should be considered when selecting the instrument.
Grasping instruments are sometimes used to stabilise tissues away from the surgeon’s field or for easier tissue handling. Some of these instruments have a locking mechanism that enables the tissue to be grasped without continuous action from the surgeon. They should be used judiciously and should not be allowed to remain on tissues for longer than necessary. Common examples include the use of Allis tissue forceps to hold the linea alba during an ovariohysterectomy or laparotomy, Babcock tissue forceps to hold the urinary bladder during cystotomy and Doyen intestinal forceps for intestinal anastomosis. See Unit 9 Topic 2b
Retraction can be achieved with appropriate instruments, packing or stay sutures. Minimal trauma to the retracted tissues must be a primary goal. The common practice is to protect the tissues with a moistened laparotomy sponge before the retractor is applied
Retractors can be hand-held or self-retaining. The latter is indispensable if the surgeon is working without a sterile assistant. However the tendency to leave a self-retaining retractor on tissues for a prolonged period of time should be avoided. Excessive retraction pressure should not be applied, to avoid ischaemia at the point of contact. See Unit 9 Topic 2c
Stay sutures are relatively atraumatic and serve to stabilise and manipulate the tissue. More than one stay suture can be use. This minimises the number of instruments in the surgical field. Stay sutures can be anchored to drapes or weighted over the incision by an instrument such as a haemostat to free the surgeon. Size 2-0 monofilament suture material is least traumatic. Common examples include stabilising the stomach or urinary bladder during exploration. Stay sutures can also be used to create a pericardial basket during cardiac procedures or to retract the dura after a durotomy to inspect the spinal cord.
Moistened sponges are particularly useful for packing off structures that creep into the surgical field. Common examples include packing of intestinal loops or lung lobes. Sometimes moistened sponges are packed behind the target organ to displace it towards the surgical field. An example of this is packing moistened sponges between the diaphragm and the liver for better exposure of a liver lobe. Remember to remove the sponges at the end of the procedure.
Retraction using tissues at the surgical site can be effective in selected circumstances.

The mesocolon is commonly used to retract abdominal viscera to the right to gain exposure of the left kidney or a loose ligature of the left ovarian stump. Similarly the mesoduodenum can retract viscera to the left to gain exposure of the right kidney.
4.Tissues must be kept moist during dissection
Allowing tissues to dry will result in an inflammatory response and potentiates adhesions between tissues such as the intestines. It is important that all exposed tissues such as serosa be kept moist with warm sterile saline.
5. Avoid transection of muscle bellies.
Deeper exposures may need incision of fascia or sub-periosteal elevations of origins or insertions of muscles.
6. Keep operative time to minimum
`Time is trauma' (Vasseur 1985). In human surgery, the rate of postoperative infections following a 90 minute procedure is twice that of a 60 minute procedure.
The rate of infection doubles for every hour of surgery.
7. Close “dead space”
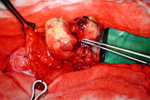
“Dead space” can be defines as the cavity left in the tissues after the closure of a wound. An example of this is the space left behind in the tissues following the removal of a space-occupying tumour such as a lipoma (benign fatty tumour) in the subcutaneous tissues.
Image <removal of lipoma>
This space allows the accumulation of serum (seroma) or blood (haematoma) which both slow the healing process and potentiate infection of the surgical wound as a result of reduced defense mechanisms within the fluid-filled space, and the bacterial friendly environment.
Dead space should be surgically closed, or evacuated with a mechanical drain.
8. Reduce the amount of foreign bodies within the wound
The presence of materials foreign to the body eg. suture material, bone plates and pins, significantly increases the incidence of surgical infections. Depending on their properties they may also influence healing in the local environment of the implant (see Unit 7).
9. Be aware of the number of instruments, swabs and other equipment that you are using during surgery.
In a 35 year study in Canada over 300 pieces of surgical gear were accidentally left inside human patients including swabs, needles, catheters, forceps etc. Retained packs in humans have been reported as having a 25% mortality.
10. Adequate knowledge of surgical instruments.
Gentle tissue handling can be achieved by selecting the appropriate instrument and using it for its designated purpose. The use of inappropriate instruments is potentially the most common cause of tissue injury during a surgical procedure. See Unit 9
11.Maintain visualization of the tissues
It is essential to maintain good visualization of the tissues you are working on. This can be achieved by adequate retraction of adjacent tissues, lavage (flushing) with warmed saline and suction, and the use of good haemostatis (see below).
12. Adequate haemostasis
Inadequate haemostasis will both obscure the surgical field, prolonging the surgery and potentiate the development of a haematoma at the surgical site. See Topic 4

 Neo loops
Neo loops
 Moist packs in abdomen
Moist packs in abdomen


