The Patient
Unit 4: Preoperative Assessment & Management
Topic 3: Diagnostic Techniques
The use of additional testing and diagnostic methods are usually dictated by the presenting signs, differential diagnostic list, type of surgery being considered and experience of the clinician. They may be classified as either indirect or direct methods.
Indirect methods
a) Haematology/Biochemistry
Laboratory examination of blood and urine samples from the patient can contribute significant information prior to surgery. Whilst these tests are infrequently performed prior to short routine procedures they should be undertaken if either the procedure is likely to be prolonged or extensive, or if the animal is aged (over 10 years of age), irrespective of the animals clinical condition.
At the University of Melbourne the routine “preanaesthetic screen” includes haematocrit, total protein, blood urea nitrogen, ALT, AP and a full urinalysis.
In more complicated cases the tests chosen will depend on the condition being evaluated.
Alternatively, full profiles usually include electrolyte analysis (Na, K and Cl). Most testing laboratories have standard profiles from which to select.
Urinary tract:
- urea
- creatinine
- urine analysis
- serum electrolytes
Liver function tests:
- coagulation profile
- ALT, ALP
- Bilirubin (conjugated vs unconjugated)
- Albumin
Coagulation profiles and a buccal mucosal bleeding time assessment may be useful if a clotting deficiency is suspected on the basis of the patient’s history, or its breed.
For example, Dobermann Pinschers have a high incidence of von Willebrand disease. The Buccal Mucosal Bleeding Time (BMBT) is a useful presurgical test of haemostatic competency as it evaluates the entire primary haemostatic system (vessel wall and platelet function). This test makes use of a cutting instrument (e.g. Surgicutt - International Technidyne Corp.) to make a small incision in the buccal mucosa. The time for haemostasis to occur is then recorded. Normal range is 2.6 +/- 0.5 minutes for dogs and 1.9 +/- 0.5 minutes for cats. Blood smears may be useful in quantitatively evaluating platelet numbers. Acceptable: > 3-5 platelets per high power field.The secondary haemostatic mechanism involves a cascade of enzymatic reactions resulting in the formation of a stable fibrin clot by the circulating coagulation factors. Factor VIII deficiency in German Shepherds is an example of problems associated with this mechanism.
To evaluate the coagulation cascade, blood should be collected into citrated siliconised collection tubes. The samples are evaluated for PT (prothrombin time) and APTT (activated partial thromboplastin time). PT evaluates the extrinsic and common pathway, whilst APTT evaluates the intrinsic and common pathways (including factor VIII).
An activated clotting time (ACT) may also be performed to evaluate the intrinsic and common pathways. It is performed by collecting 2 mL of blood into a pre-warmed diatomaceous earth container which is then incubated at 37°C. The sample is examined every 10-15 seconds to observe clot formation. Normal ACT: 60-125 seconds.
b) Urinalysis, including examination of the sediment.
This is particularly important in assessing renal function in animals receiving drugs (e.g. non-steroidal anti-inflammatory analgesia) that are metabolised or excreted by the kidneys. It is also essential prior to urinary tract surgery.
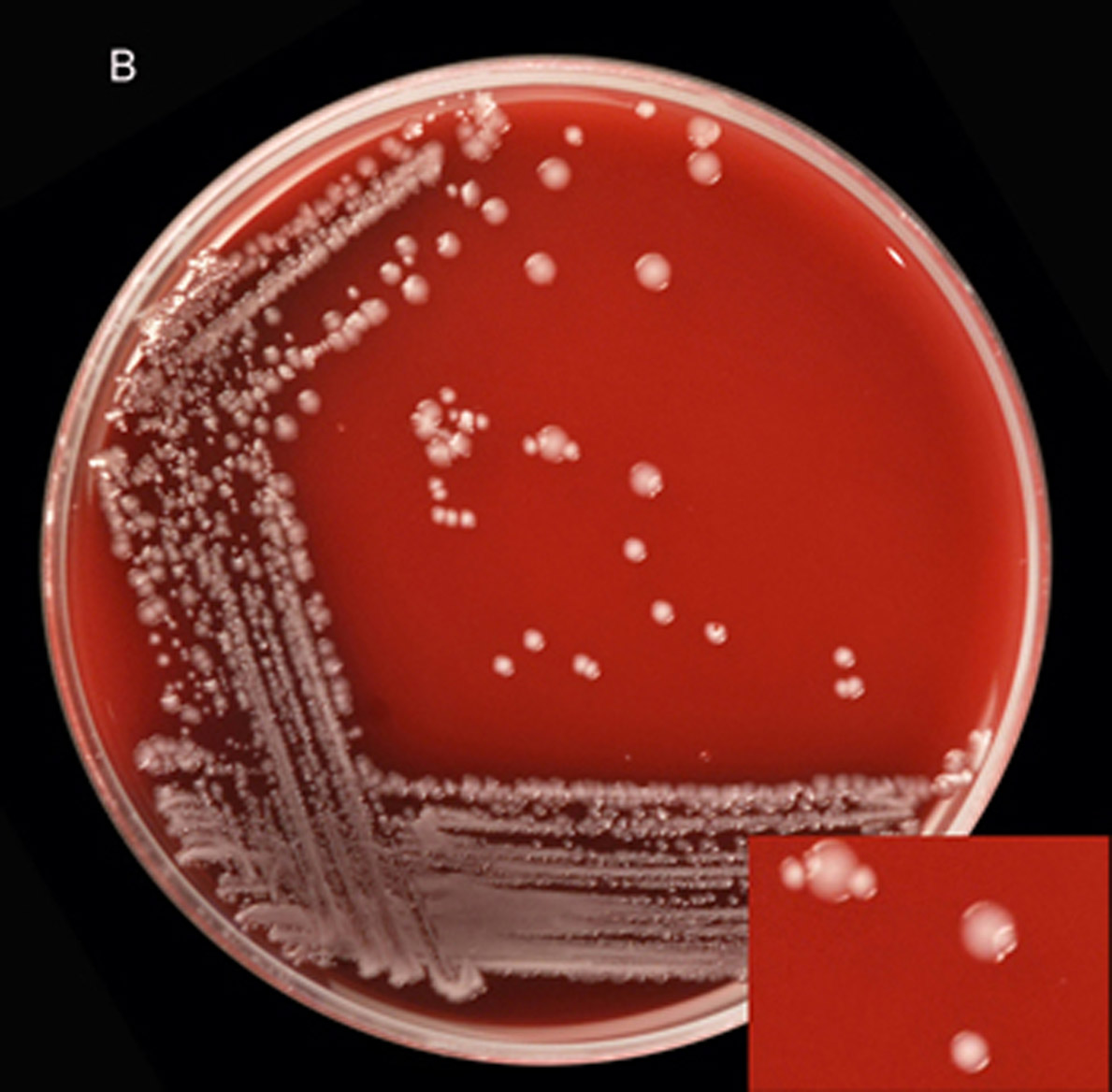
c) Microbiology (Culture and Sensitivity testing)
Managing pre-existing infections with appropriate antibiotics can be very useful in managing the spread of infection in some procedures such as ear surgery.
d) Diagnostic imaging
Radiographs, plain and contrast
Radiographs taken with X-rays were the first source of radiation to be used in diagnostic medicine. They were discovered by W. Roentgen in 1895 with standard machines found in most veterinary practices operating at voltages of around 15-200kV.
At these voltages the dominant mechanism for energy loss by the X-rays is the photoelectric effect. This effect is strongly dependent on atomic number, and as there is a substantial difference between the atomic number of elements present in bone (Z=14), and soft tissue (Z=7), bone will absorb X-rays much more strongly than soft tissue.
The X-rays that manage to penetrate through the patient’s body will fall on the photographic film within the film cassettes.
In those situations were there is little difference between the Z-number of the tissues, the image can be improved by the use of a contrast medium which frequently consists of either barium sulphate or iodine which have a high Z number and therefore absorb the X-rays much more strongly than the surrounding tissues, thereby providing a contrast between tissues in which they are present.
In another X-ray technique called fluoroscopy, a real-time dynamic image is created on a TV monitor. X-rays that have passed through the patient fall on a fluorescent screen and visible light is emitted. The photons cause the emission of electrons from a photosurface, which are accelerated by a potential difference so that they fall on a second fluorescent screen from which they cause emissions of light that is fed into the TV monitor.
The advantage or real-time images are however, outweighed by the high doses of radiation required during the process. This technique is usually limited to short bursts such as used during angiography, myelography and some orthopaedic pin placements when real-time images are useful in performing the exercise.
Ultrasonography
Ultrasound is sound that cannot be detected by the human ear. The ultrasound used in diagnostic imaging is in the range of 1 to 10 MHz.
It has the advantage of not depositing X-rays into the body, but the image is generally less detailed, and can only be used to image soft tissues. The ultrasound is emitted toward the patient in short pulses (typically lasting around 1µs) and their reflections of various organs are detected.
Resolution is dependent on the wavelength provided by the ultrasound head. A 10MHz ultrasound has a wavelength of about 0.15mm, and can ‘see’ objects down to 0.15mm.
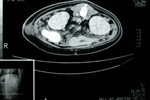
Computed Tomography (CT)
In 1973, the use of X-rays in a technique called Computed tomography (CT scan) revolutionized diagnostic imaging. It is gradually becoming more widely available in veterinary referral practices.
A movable source of X-rays emits a narrow beam that is confined to one plane and travels through the patient’s body so that it is received by multiple detectors on the other side. As the source rotates around the patient the beam enters the body from a different angle. The detectors record the intensity of the X-rays reaching them and the information is sent to a computer which analyses the data and constructs a two-dimensional image representing a cross-section of the patient.
CT images are viewed on a monitor as they are acquired and can be printed onto a film for viewing on a light box.
During the scan the X-ray tube continually revolves around the patient as the patient is moved through the aperture of the scanner. The patient is moved either in a series of small increments (axial scan mode) or continuously (helical scan mode). The size of the area to be scanned and the thickness of the image slices (as small as 1mm) can be determined by the radiographer.
The size of the aperture limits the use of CT to small animals, and the extremities of larger animals.
Magnetic Resonance Imaging (MIR)
Magnetic resonance imaging is based on a phenomenon known as nuclear magnetic resonance. It does not use X-rays and is particularly useful for detecting soft-tissue lesions, and in particular the brain and spinal column.
The system makes use of a strong magnetic field and a radio-frequency source of electromagnetic radiation to send protons into a higher energy level. This is followed by a transition down again with an accompanying emission of a photon of the same frequency. Detectors can record these photons and an image is computer generated. The rate of these transitions varies between tissue types, thus allowing the identification of tissue type.
Whilst most human hospitals use a large MIR machine, smaller, but less powerful machines are manufactured for veterinary use.
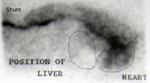
Nuclear scintigraphy (Gamma cameras)
Radioisotopes can be used as a diagnostic tool and to monitor specific body organs and their function.
Most commonly, the radioisotope technetium-99, a long-lived isotope (half-life of 6 hours) which decays by gamma emission.
This energy is readily detected externally with a detector called a ‘gamma camera’.
Technetium is useful in diagnostic studies of most body organs, such as the heart, the lungs and the liver. It is also useful for detecting active calcium absorption by bones.
Iodine-131 is used in blood volume measurements and in studies of thyroid gland function.
Thalium-201 is used in studies of muscle function and disease.
An advantage of technetium is that it is readily combined with other compounds which have an affinity for the target tissues. The radioactive compound so formed is called a radiopharmaceutical.
This is administered to the patient via a number of routes, and the radiation emitted by the technetium is recorded by the detector placed over the relevant part of the patient’s body. The amount of radiation compared with the amount expected from a healthy body then provides information about the function of that particular part of the body.
An example of this technique is the use of the trans-colonic administration of technetium pertechnetate for the diagnosis of porto-systemic shunts in dogs.
A disadvantage of this imaging mode is the need to isolate the animals and collection and isolation of their urine and faeces for a period of time until the radioactivity decreases to safe levels.
Direct methods
a) Biopsy, Cytology
- Impression smears
- Fine needle aspirates
- Needle biopsies
- Wedge biopsies
- Excisional biopsies
b) Endoscopy
Endoscopy (minimally invasive surgery) can be an extremely useful tool in the diagnosis of surgical conditions, as well as their management. It is particularly useful in isualizing and obtaining a biopsy of a lesion. A variety of endoscopes are now available to the veterinary practitioner.
- Rigid scopes e.g. rhinoscopes, otoscopes, cystoscopes, laparoscopes and arthroscopes
- Flexible scopes e.g. gastroscopes, proctoscopes
c) Exploratory Surgery
With the availability of advanced diagnostic techniques, true exploratory surgical procedures to reach a diagnosis are less common nowadays, but are occasionally required to diagnose and manage some conditions or to obtain biopsies from a variety of tissues.

“It is better to perform a negative exploratory surgery than to perform a positive post-mortem”

Articles for Information:
- Carsten, E.A. & Gilson, S.D. (2000) Endoscopy in Small Animal Medicine and Surgery. The Compendium 22, 321-324.
- Remedios, A.M. & Ferguson, J. (1996). Minimally Invasive Surgery: Laparoscopy and Thoracoscopy in Small Animals. The Compendium 18, 1191-1199.