The Patient
Unit 7: Wound Healing & Management
Topic 3: Factors Affecting Wound Healing
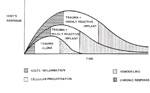
Each tissue has an optimum rate of growth in the process of healing. It is only when all the variables advantageous to healing are present, and when all the variables having the ability to disturb or retard healing are controlled or absent, that this optimum rate of growth can be achieved.
Both systemic and local factors can be important. Iatrogenic factors may also play a significant role in this!
SYSTEMIC FACTORS
Systemic disease / general patient condition
Old patients and debilitated patients have decreased capacity for fibroplasia and an increased risk of infection.
Significant disease processes such as uraemia, Cushing’s disease or disseminated cancer, can delay wound healing.
Many diseases that interfere with peripheral circulation eg. heart failure, can also significantly delay wound healing. Diabetes may cause microangiopathies but these are not a commonly recognised complication of diabetes in domestic animals but are very important in wound healing in humans.
Stress may result in the release of endogenous ACTH and cortisol. Chronic anaemia (<20%) may also delay healing due to chronic hypoxia of the tissues.
Protein deficiency
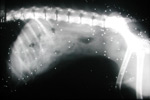
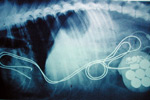
Protein deficiency may result from severe parasitism, undernutrition, malabsorption and liver disease. Serum protein levels of <6.0gm/dl may slow healing.
Lack of protein prolongs the lag phase and prevents the onset of the fibroblastic stage as the deficiency reduces collagen and proteoglycan production by the fibroblast.
Skin temperature
Increases and decreases in blood flow to a wound may influence the rate of wound healing. Reductions in skin temperature will result in vasoconstriction and reduced blood flow and therefore oxygen supply to a region. Temperatures of 12oC can result in a 20% in the tensile strength of a wound.
Hormones
ACTH, cortisol and corticosteroids (and stress leading to a release of these endogenously) inhibit both early and late phases of wound healing (inflammation, neovascularisation, fibroplasia, collagen formation, wound contraction). This may be of significant importance clinically.
Anti-inflammatory drugs
Normal therapeutic doses of NSAIDs appear to have little effect on normal wound healing. It has recently been reported that flunixin meglumine delayed wound healing in rats and horses but reports are conflicting. Certainly, these drugs are commonly used as analgesics and anti-inflammatories with no untoward clinical effects.
However, corticosteroids certainly have an adverse effect on wound healing.
Cytotoxic drugs
The action of these drugs is to interfere with cell proliferation. Use of these agents may delay wound healing, and their use post tumour removal is generally delayed until the surgical wound has healed.
Nutrition
Optimum wound healing cannot occur without adequate nutrition. Protein malnutrition impairs immune function as well as wound healing.
A vital component in managing wounds therefore is the nutritional support of the patient. It has been well documented that early enteral feeding improves wound healing.. Nasogastric, pharyngostomy and gastroenterostomy tubes may be required if the patient is unable or unwilling to eat.
Diets formulated specifically for the hypermetabolic state of patients with severe injuries are available (A/D diet - Hills Pet Nutrition Ltd, ClinicareTM - Pet-Ag Inc.).
LOCAL FACTORS
Trauma
Excessive trauma and wound contamination increases the amount of debris in a wound and may decrease the viability and activity of the affected tissues. Therefore the first stages of healing are prolonged and the rate of gain of tensile strength is decreased.
The possibility of infection is also increased due to the presence of debris, serum, devitalised tissue and a decreased blood supply to the area.
Excessive scar production can also occur.

The experience and skills of the surgeon can be the most influential factor in determining the extent of surgical trauma suffered by the patient.
A number of surgically related factors will influence the degree of tissue injury. These are described in the tissue handling section of the intra-operative considerations.
Link to Tissue Handling Unit 6, Topic 1
Motion
Excessive motion disrupts the organisation of budding capillaries and fibroblasts.
It can lead to excessive collagen production and unsightly scars.
Nevertheless, an appropriate amount of continuous passive motion has been shown experimentally to allow collagen to organise along tissue stress lines and to promote earlier tensile strength of wounds.
Decreased blood supply
This may be the result of:
- injury to regional vessels eg. directly by traumatic surgery; by tight sutures etc.
- pressure of old or new scar tissue
- application of tight bandages, casts and splints.
All of these can lead to poor local oxygen gradients.
Although tissue hypoxia within the wound is a potent stimulation for neovascularisation, regional blood supply needs to be maintained for continued healing.
Improper closure of wounds
Tissue layers in a wound should be closely apposed. The formation of tissue `steps' should be avoided.
Eliminating dead-space is important. Accumulation of blood and serum within dead space will physically separate tissue and can be an excellent nidus for infection.
Conversely, the overenthusiastic use of suture material can lead to irritation and increased bulkiness of the wound.
Free fluid in wounds
Accumulation of clotted blood and serum between tissue layers prevents proper apposition of tissues. The formation of a haematoma within the wound can cause pressure sufficient to interfere with blood supply.
Free fluid in a wound also encourages bacterial growth.
A seroma is the post-operative accumulation of serosanguinous fluid. It can occur when:
- dead-space is not reduced or drained;
- lymph vessels have been transected;
- here is movement in the wound;
- excessive foreign material is present;
- there is poor haemostasis.
Infection
The mere presence of organisms within a wound does not necessarily mean that infection and subsequent delayed healing will result. For most pathogens, a concentration of 105 organisms per gram of tissue is necessary to produce an infection. The presence of dead tissue, foreign material, dead space, fluid etc. will hasten the progression of an infection. Good surgical technique is more important for good wound healing than any other factor (prevention is better than cure). Despite this, there is no doubt that delayed healing is an important consequence of wound infection.
Infection delays wound healing by separating the wound edges, prolonging the natural debridement stage and by producing further tissue damage.
Temperature
In general higher temperatures promote healing. Cold may result in vasoconstriction, a decrease in the oxygen and nutrient supply to a wound and slower healing.
30°C appears to be the optimal temperature for wound healing.
Foreign bodies
Wounds rarely heal if a foreign body within a wound causes a chronic irritation or becomes infected. Not all foreign bodies cause problems however. For example, polished, non-porous metal eg. plates and screws can sit in tissues without causing a problem for the life of the host.
Foreign bodies can be divided into 2 main groups:
- Those that are accidently placed into the wound.
- Those that are deliberately placed into the wound
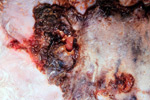
Accidentally placed foreign bodies
The bodies response to these materials will depend greatly on the type and reactivity of the material. In general, inert materials such as glass, carbon, lead shot etc, if not greatly contaminated will remain in the body without causing problems. The body will wall off ("encapsulate") the material with fibrous tissue.
The presence of organic materials such as grass seeds, soil, surgical glove powder (starch) etc on the other hand will result in a vigorous and ongoing inflammatory reaction. The wound will not heal, and typically discharges through an open sinus. It is important that these materials are removed for the wound to heal.
Deliberately Placed Materials
A wide variety of materials with diverse properties have been deliberately or surgically placed into the body. They are made of substances that are relatively inert or that stimulate a biological response, and either temporarily or permanently assist or assume the function of a body part. These materials are loosely termed "biomaterials", and include suture materials, meshes, orthopaedic implants (Plates, pins, screws), haemostatic agents, cardiac pacemakers and heart valve replacements.
Biomaterials can therefore be classified in a number of ways:
- synthetic/biological
- absorbable/non-absorbable
- reactive/non-reactive
A considerable amount of research has, and continues to be conducted into better understanding the body’s response to various materials in order to improve implant performance.
Implantation of a biomaterial involves surgical trauma at the implant site. In general, all foreign materials within a wound result in an enhanced inflammatory response, the type and extent of which is determined by a number of factors. These will influence the type of protein absorption onto the surface of the material in the immediate period following implantation - called the interface conversion.
In general, if albumin is the predominant protein absorbed onto the surface of the material, then "surface pacification" will usually occur in which all cells around the material will remain rounded, and non adherent with little cellular reaction. The implant will become encapsulated by a thin wall of dense collagenous material whose individual fibres are aligned parallel to the implant surface.
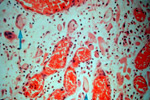
If, on the other hand, fibronectin or vitronectin is absorbed onto the surface, then there will be strong cellular adhesion to the material and a much more vigorous reaction. The inflammatory phase may become chronic, and persist with the presence of a large number of macrophages. As a unique response to foreign materials causing a chronic inflammatory reaction, there is the formation of foreign body giant cells by the fusion of macrophages, which may appear as soon as 4 days post implantation. Whilst this "foreign body reaction", in which macrophages and foreign body giant cells exist at the material interface may persist for the lifetime of the implant, the subjacent implant site may undergo fibrous tissue proliferation and fibrosis.
Thus there may be great variations in the number and types of cells, the duration of the cellular activity, the size of the tissue reaction zone and the final capsule thickness as a consequence of the type of interface conversion occurring in response to the implanted material.
Factors influencing this interface conversion include:
- The chemical composition and degradation of the material
- The surface free-energy (wettability) of the material
- The shape and porosity of the material
- The implant site
- The mechanical properties of the material, and the adjacent tissues
- Infection
- Species of animal
- Age of the host Sex of the host.
Generally the greater the reactivity of the implant material, the longer and more vigorous will be the host response.
The presence of a foreign body, including suture materials, always increases the chance of infection within a wound.
In a classic experiment in humans, the number of Staphylococcal pyogenes bacteria required to cause infection in a wound was reduced from 1 million to 100 in the presence of a single silk suture. The potential for converting contamination within a wound to infection, and the degree of infection, however does depends on a number of factors:
- the physical make-up of the suture
- the sutures ability to induce an inflammatory reaction
- the chemical structure, capillarity, fluid absorbency and bacterial adherence to a suture.
- the number of bacteria present
- the surgical technique
- the host resistance to infection.
A description of the suture types available, and their properties are detailed in Unit 11.
Hyperlink to Unit 11 (sutures)
There are therefore a number of possible fates for an implanted biomaterial.
It may be:
- absorbed
- removed
- encapsulated
- extruded
- or persist as a continuous focus of inflammation

Swaim, S.F., Hinkle, S.H. and Bradley, D.M. (2001) ‘Wound contraction: basic and clinical factors’. Compendium 23 (1) 20-33.